Truth—perimenopause and menopause can feel like your body is playing a trick on you.
One minute you’re fine, and the next, your joints, muscles, and even bones seem to have their own agenda. Women in perimenopause and menopause can experience tendon and ligament injuries that seem to last forever, frozen shoulder, plantar fasciitis, and random joint pain. Ever wonder why? It turns out, estrogen receptors are everywhere in the body, especially in the musculoskeletal system. Notably, these receptors are found in muscles, tendons, ligaments, joints, and bones, which means estrogen plays a critical role in keeping these tissues healthy and functional. As estrogen levels fluctuate and then drop during perimenopause and post menopause, it affects everything from muscle mass to joint flexibility, leaving us more prone to aches, stiffness, and even injury. But here’s the good news—you can take steps to mitigate these changes and stay strong, mobile and injury-free.
Muscles: Keeping Your Strength in Check
Estrogen doesn’t just influence reproductive health—it also helps regulate muscle maintenance and repair. Estrogen receptors in the muscles support protein synthesis, which helps build and repair muscle tissue. With lower estrogen, you might notice muscle weakness, loss of muscle mass (called sarcopenia), or increased fatigue.
However, this muscle loss isn’t irreversible—by focusing on strength training and protein intake, you can maintain your muscle mass and energy levels.
- What to do: Aim for two to three resistance training sessions per week, targeting major muscle groups like your legs, arms, and core. Exercises like squats, deadlifts, and push-ups are your go-to.
- Why it helps: Strength training stimulates muscle growth, helps preserve muscle mass, and combats the decline in strength that can happen with menopause.
- Protein Power: Boost your protein intake to 20-30 grams per meal. This supports muscle recovery and synthesis, helping to offset muscle loss.
- Helpful Hints – Try high-quality protein sources like eggs, lean meats, tofu, cottage cheese, fat-free Greek yogurt, legumes at each meal for sustained muscle support.
Consider working with a certified trainer who understands menopause and can customize a strength training program for you to target muscle retention and ease joint discomfort.
Tendons and Ligaments: Flexibility and Stability Challenges
Tendons and ligaments, which connect your muscles and bones, also rely on estrogen to stay flexible and strong. Estrogen receptors in these tissues help maintain their elasticity, so when estrogen levels drop, tendons and ligaments become more rigid and prone to injury. You might notice more stiffness in your movements or even discomfort during physical activity.
- What to do: Prioritize dynamic stretching before workouts and joint-stabilizing
exercises to protect these connective tissues. - Why it helps: Dynamic stretches—like leg swings or arm circles—improve flexibility
and warm up your joints and tendons for activity. - Balance Work: Include exercises that target balance and stability, like single-leg squats or using a stability ball. These strengthen the smaller, supportive muscles that
protect tendons and ligaments.
Joints: Tackling Inflammation and Pain
Estrogen plays a protective role in the joints by reducing inflammation and helping to maintain joint lubrication. As estrogen declines, joint pain, stiffness, and even inflammation can increase, particularly in areas like the knees and hips. This is why many women experience aching joints during and after menopause.
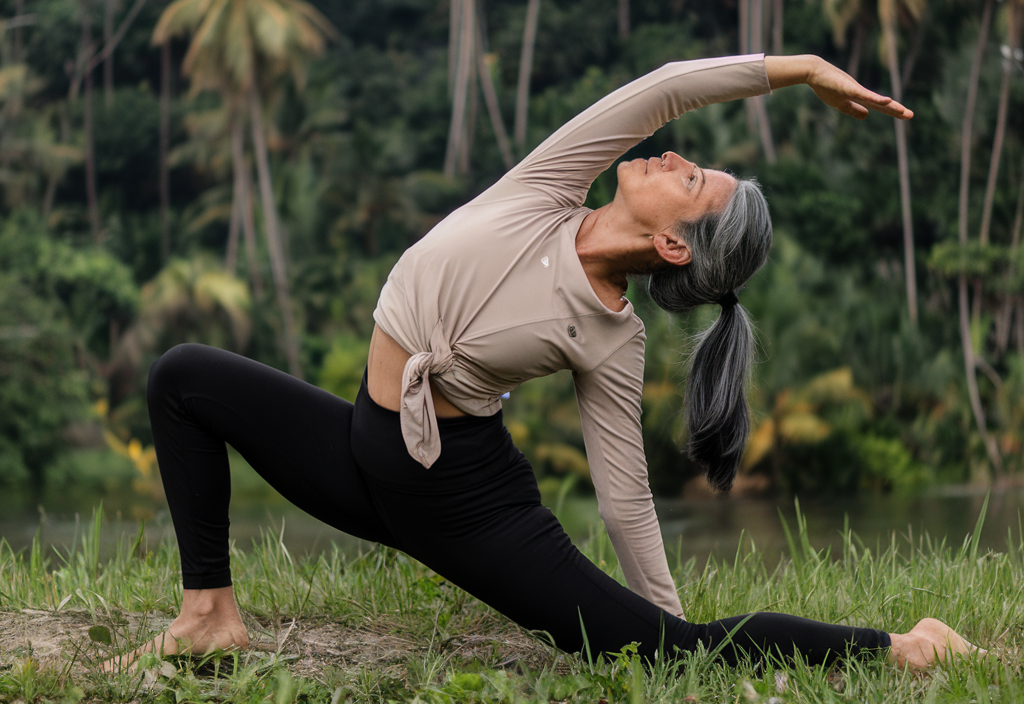
- What to do if you are particularly achy: Stick to low-impact activities like swimming, cycling, or yoga, which provide exercise benefits without putting
- Why it helps: Low-impact exercises keep you active without worsening joint
inflammation. - Anti-inflammatory Diet: Load up on omega-3-rich foods (like salmon, flaxseeds, and
walnuts) and antioxidants from berries and leafy greens to help combat inflammation and protect your joints. - Helpful Hints – Omega-3s have been shown to lower inflammation levels in the body, reducing joint pain and improving flexibility. Do your best to avoid highly processed
foods and those with added sugar.
Bones: Maintaining Density and Preventing Fractures
Your bones are particularly vulnerable to declining estrogen levels. Estrogen helps regulate the balance between bone formation and breakdown, so when its levels fluctuates as in perimenopause and then drops as it does in menopause, bone loss accelerates—a major risk factor for osteoporosis. Estrogen receptors in the bones ensure proper calcium absorption and bone turnover, so it become even more important that women focus on maintaining bone density during and after menopause.
- What to do: Incorporate weight-bearing exercises like walking, hiking, AND consistent resistance training 2-3 x week, AND high-intensity interval training 2 x week, to stimulate bone growth.
- Why it helps: These activities encourage bone formation, helping to slow down the
bone loss associated with estrogen decline. - What to do: Ensure you’re getting 1200 mg of calcium split over 3 to 4 servings daily
and around 1000 IU of vitamin D daily, preferably through food, though many women need to supplement with vitamin D. - Where to find it: Load up on dairy, fortified plant-based milks, leafy greens, and fatty fish like salmon to meet your daily needs.
Taking Action: Staying Strong Through Menopause
Menopause doesn’t have to mean losing your strength, flexibility, or vitality. By understanding how estrogen impacts your muscles, tendons, ligaments, joints, and bones—and by incorporating targeted exercises, a nutritious diet, and the right supplements—you can stay active and resilient. Embrace these strategies to thrive through menopause and beyond, and remember, your body may change, but with the right approach, you can stay strong, mobile, and injury-free.
~ Dr Jen Burke
MD, CAQSM, DipABLM, NBC-HWC
thePause™ Board of Medical Advisors